Why System Integration Matters in Clinical Environments
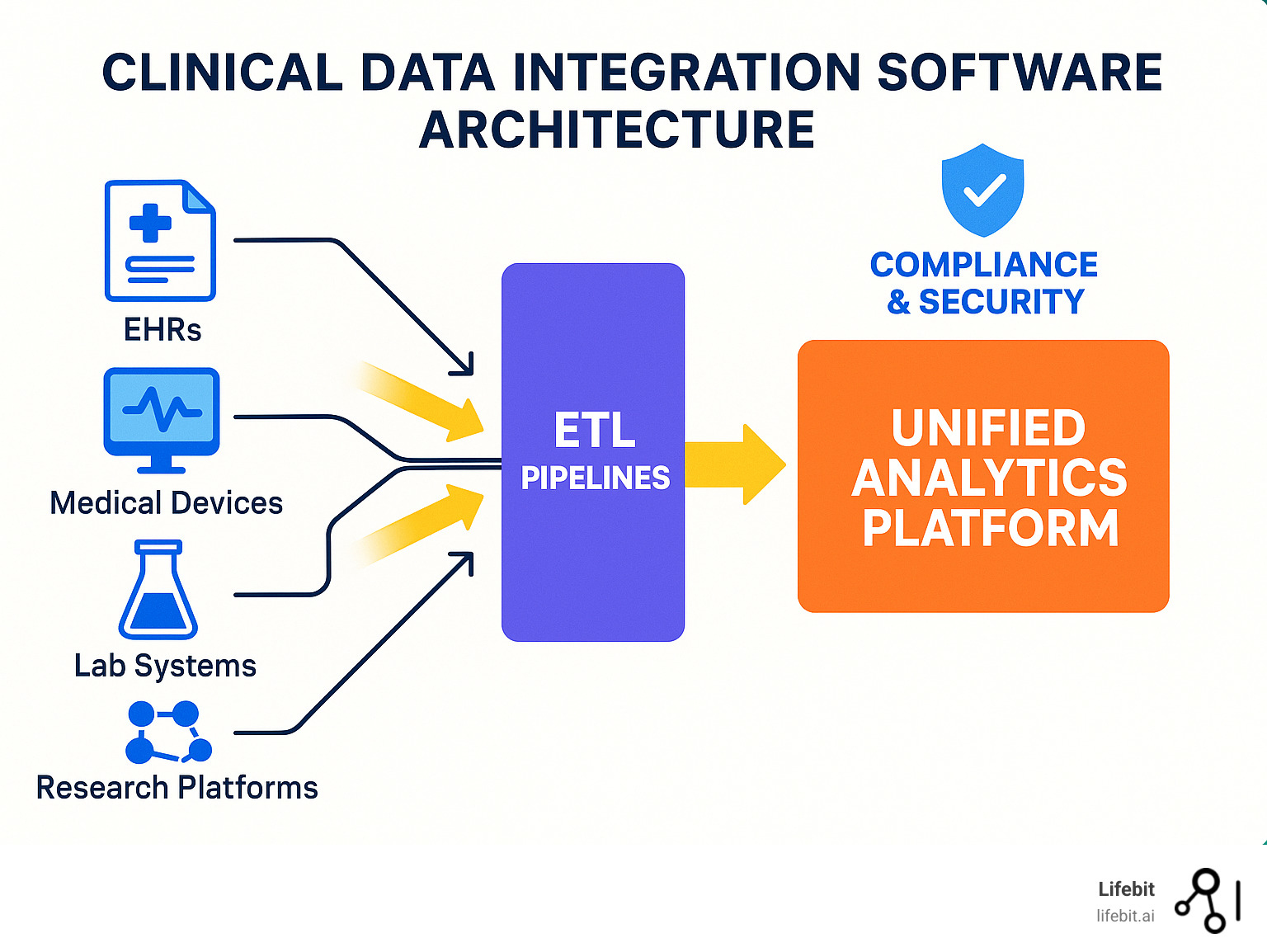
Modern clinical environments depend on a wide range of technologies operating simultaneously. Diagnostic imaging systems, patient monitoring devices, laboratory analyzers, electronic health records, pharmacy systems, and clinical decision-support tools all contribute to patient care.
Each of these technologies generates critical data that informs diagnosis, treatment planning, and ongoing patient management. When systems operate independently, this information becomes fragmented, forcing clinicians to piece together incomplete or delayed data during time-sensitive situations.
System integration ensures that information flows seamlessly across departments and platforms, supporting coordinated, informed, and timely clinical decision-making. In high-pressure healthcare settings, integration is not about convenience—it directly influences patient safety and outcomes.
The Complexity of Clinical Ecosystems
Hospitals function as complex ecosystems where patients move continuously between departments such as emergency care, diagnostics, surgery, intensive care, and recovery. Each transition introduces opportunities for information loss if systems are not properly connected.
Clinicians rely on shared access to patient histories, test results, imaging data, medication records, and real-time vital signs. Fragmented systems force healthcare professionals to switch between multiple interfaces, manually re-enter data, or rely on verbal handovers that increase the risk of miscommunication.
Integration connects devices, software platforms, and data repositories into a unified clinical environment. This unified approach reduces operational friction, improves situational awareness, and allows care teams to focus on clinical judgment rather than system navigation.

Enhancing Patient Safety
Patient safety depends on accurate, timely, and complete information. Integrated systems reduce manual data entry, lowering the risk of transcription errors that can lead to incorrect diagnoses, medication errors, or delayed treatment.
Real-time data synchronization allows clinicians to respond quickly to changes in patient condition. Alerts generated by integrated monitoring systems can signal early warning signs, enabling intervention before complications escalate.
In high-acuity settings such as intensive care units and emergency departments, integration ensures that life-critical information is available instantly, supporting faster and more confident clinical decisions.

Operational Efficiency and Staff Experience
Beyond patient safety, system integration plays a vital role in operational efficiency. Integrated workflows eliminate duplicate documentation, reduce administrative workload, and streamline coordination between departments.
Clinicians spend less time managing disconnected systems and more time engaging directly with patients. This efficiency improves care quality while also addressing staff fatigue and burnout, which are growing challenges in healthcare systems worldwide.
A well-integrated clinical environment supports smoother shift handovers, clearer accountability, and improved collaboration across multidisciplinary teams.
Preparing for Future Healthcare Demands
As healthcare technology continues to evolve, system integration becomes even more critical. Advanced technologies such as artificial intelligence, predictive analytics, telemedicine, and remote patient monitoring rely on continuous data exchange across platforms.
Organizations that invest in integration today create a flexible foundation capable of supporting future innovations without disrupting existing operations. Integrated systems allow healthcare facilities to scale, adapt, and innovate with confidence.
Without integration, adopting new technologies often adds complexity rather than value. Integration ensures innovation enhances care rather than complicating it.
Conclusion
System integration is not a technical luxury—it is a clinical requirement in modern healthcare environments.
By unifying technologies into cohesive, interoperable systems, healthcare organizations enhance patient safety, improve operational efficiency, and build resilient infrastructures capable of meeting future clinical challenges.

Leave a Reply