The Importance of Lifecycle Planning in Medical Equipment
Medical equipment represents one of the most significant and long-term investments within healthcare organizations. From diagnostic imaging systems to life-support technologies, these assets directly influence patient outcomes, operational efficiency, and regulatory compliance.
Despite this importance, equipment decisions are often approached as isolated purchases rather than components of a comprehensive lifecycle strategy. Without structured planning, hospitals risk premature obsolescence, rising maintenance costs, and operational disruption.
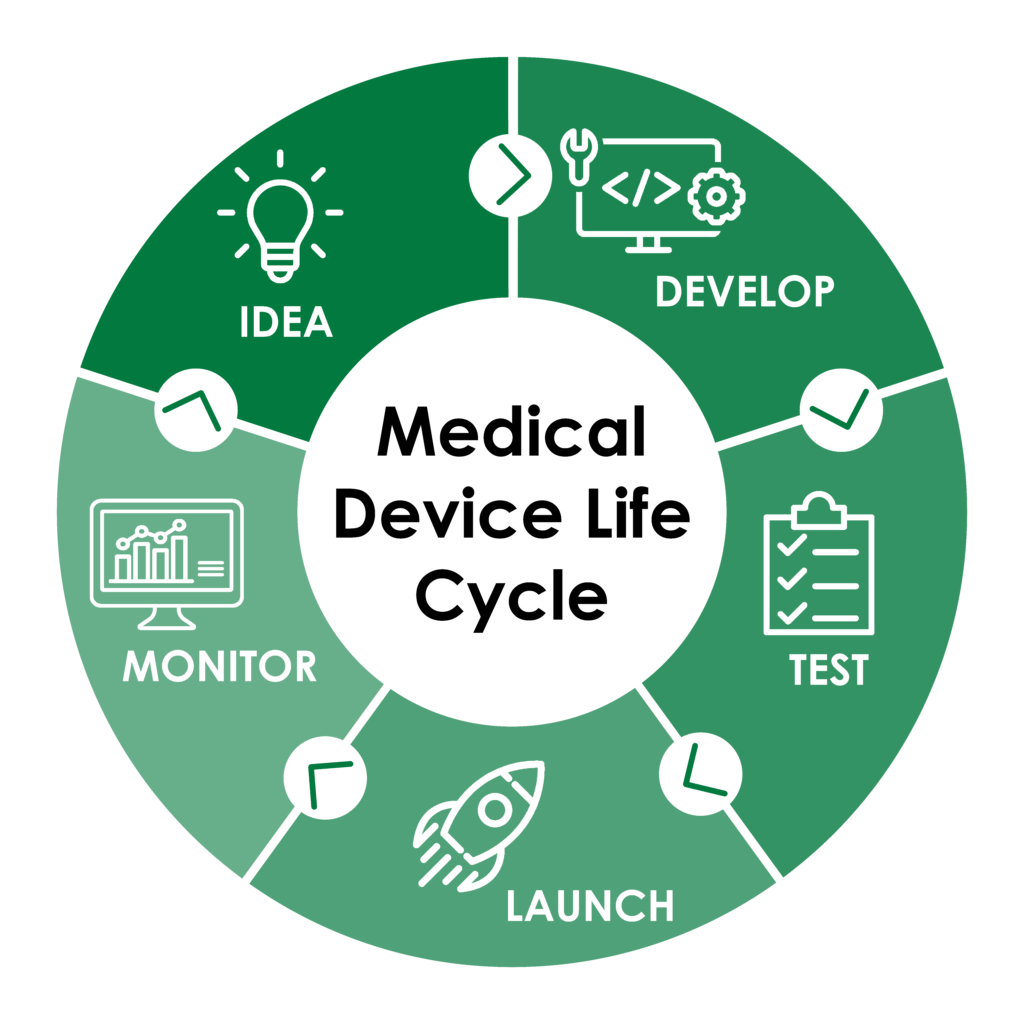
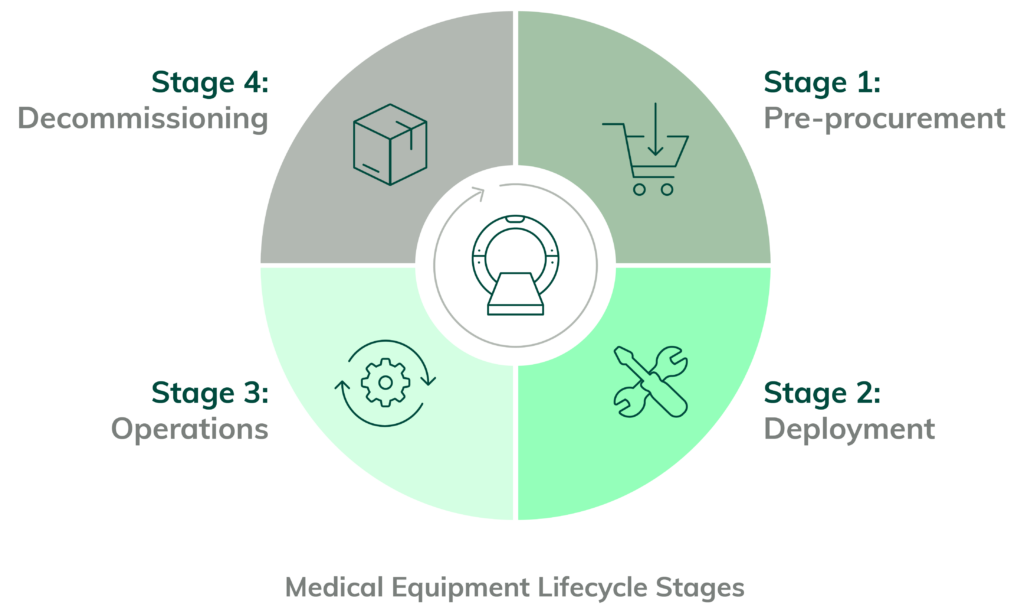
Lifecycle planning provides a framework for managing medical equipment from initial acquisition through deployment, maintenance, upgrades, and eventual replacement.
Understanding the Medical Equipment Lifecycle
The lifecycle of medical equipment begins long before installation and extends well beyond daily clinical use. It encompasses procurement, commissioning, utilization, servicing, compliance management, and end-of-life decisions.
Each phase introduces distinct technical, financial, and clinical considerations. Decisions made early in the lifecycle directly influence long-term reliability, total cost of ownership, and clinical effectiveness.
Effective lifecycle planning ensures that equipment continues to meet clinical needs while aligning with evolving standards and technologies.
Balancing Clinical Performance and Financial Sustainability
Medical equipment must deliver consistent clinical performance without placing unsustainable financial strain on healthcare institutions.
Lifecycle planning allows organizations to forecast maintenance costs, spare part availability, and upgrade requirements over time.
By anticipating these factors, hospitals can avoid reactive spending and make informed investment decisions that support both care quality and budget stability.
Ensuring Regulatory Compliance Over Time
Healthcare regulations evolve continuously, reflecting advances in technology, safety standards, and clinical best practices. Equipment that meets regulatory requirements at purchase may require updates or modifications later.
Lifecycle planning integrates compliance monitoring into equipment management, ensuring certifications, calibrations, and documentation remain current.
This proactive approach reduces the risk of non-compliance, audits, and service interruptions.

Supporting Reliability and Patient Safety
Equipment reliability is inseparable from patient safety. Failures in critical systems can compromise care delivery and delay life-saving interventions.
Lifecycle planning incorporates preventive maintenance, performance monitoring, and timely upgrades to reduce the likelihood of equipment failure.
This systematic approach ensures that technology performs as expected throughout its operational life.
Managing Technological Obsolescence
Rapid innovation increases the risk of technological obsolescence. Equipment may become incompatible with new software platforms, data standards, or clinical workflows.
Lifecycle planning evaluates upgrade paths and interoperability to extend equipment relevance without unnecessary replacement.
Planned transitions minimize disruption and protect prior investments while enabling adoption of new capabilities.

Aligning Equipment Strategy with Clinical Evolution
Clinical practices evolve alongside medical knowledge and patient expectations. Equipment must support new treatment protocols, care models, and workflow designs.
Lifecycle planning aligns technology investments with long-term clinical strategies, ensuring equipment remains fit for purpose.
This alignment strengthens the connection between technology and patient-centered care.
Conclusion
Lifecycle planning transforms medical equipment management from reactive maintenance into a strategic discipline.
By considering performance, compliance, cost, and clinical relevance across the entire equipment lifespan, healthcare organizations build safer, more resilient, and more sustainable care environments.

Leave a Reply